Could a Surprising Ally Help in the Fight Against Type 2 Diabetes?
Published: 2025-09-20 02:18:00 | Category: Uncategorized
This new study from Duke University School of Medicine reveals that pancreatic alpha cells, traditionally known for producing glucagon, also generate GLP-1, a hormone crucial for insulin regulation and glucose management. This finding challenges established beliefs about blood sugar regulation and suggests new avenues for type 2 diabetes treatment.
Last updated: 19 September 2023 (BST)
Key Takeaways
- Pancreatic alpha cells produce GLP-1, a hormone that enhances insulin secretion.
- Blocking glucagon production led to increased GLP-1 and improved blood sugar control in animal studies.
- Measuring bioactive GLP-1 accurately is crucial for understanding its role in diabetes treatment.
- Future research may focus on enhancing natural GLP-1 production to support insulin levels in diabetics.
- This discovery suggests a backup mechanism for blood sugar regulation that could transform diabetes therapies.
Understanding Alpha Cells and Their Role in Diabetes
The pancreas plays a critical role in regulating blood sugar levels, primarily through the actions of two types of cells: alpha cells and beta cells. Alpha cells produce glucagon, which raises blood sugar levels when they drop too low, while beta cells produce insulin, which lowers blood sugar by facilitating cellular uptake of glucose.
For years, the scientific community believed that alpha cells were solely responsible for glucagon production. However, the recent study from Duke University has unveiled a more complex and dynamic role for these cells. They not only produce glucagon but also have the capacity to generate GLP-1, a hormone that enhances insulin secretion and lowers blood sugar levels.
What is GLP-1 and Why is it Important?
GLP-1, or glucagon-like peptide-1, is a hormone that plays a significant role in glucose metabolism. It is released in response to food intake and helps to:
- Increase insulin secretion from beta cells.
- Inhibit glucagon release from alpha cells.
- Slow gastric emptying, which helps control postprandial (after eating) blood sugar levels.
This hormone is mimicked by several popular diabetes medications, such as Ozempic and Mounjaro, which have gained attention for their effectiveness in managing type 2 diabetes. The findings from the Duke study suggest that boosting the body's own GLP-1 production could provide a more natural approach to diabetes management.
Shifting Paradigms: The Discovery of Alpha Cell Flexibility
Led by Dr. Jonathan Campbell, the Duke research team conducted an analysis of pancreatic tissue from both human and mouse models. They discovered that human pancreatic tissue produces significantly higher levels of bioactive GLP-1 than previously recognised. This finding indicates that alpha cells are not as rigid in their function as once thought; they can adjust their hormone outputs to support blood sugar regulation effectively.
This flexibility could redefine treatment approaches for type 2 diabetes, particularly since beta cells often struggle to produce enough insulin due to insulin resistance or damage. The ability of alpha cells to switch from glucagon production to GLP-1 production offers a potential mechanism for maintaining blood sugar balance.
Insights from Animal Studies
The researchers conducted experiments on mice to further understand the implications of glucagon and GLP-1 interaction. When glucagon production was blocked, the expected outcome was a decrease in insulin levels. Contrary to these expectations, the alpha cells ramped up GLP-1 production, leading to improved glucose control and enhanced insulin release.
Dr. Campbell stated, “We thought that removing glucagon would impair insulin secretion by disrupting alpha-to-beta cell signalling. Instead, it improved it. GLP-1 took over, and it turns out, it's an even better stimulator of insulin than glucagon.” This revelation highlights the importance of GLP-1 in diabetes management and suggests that therapies aimed at increasing GLP-1 production could be beneficial.
Mechanisms Behind GLP-1 Production
The study also explored the role of specific enzymes in hormone production. Two enzymes were manipulated: PC2, which promotes glucagon production, and PC1, which facilitates GLP-1 production. By blocking PC2, researchers observed an increase in PC1 activity, leading to improved glucose control. However, when both enzymes were inhibited, insulin secretion decreased, and blood sugar levels rose, underscoring the critical role of GLP-1 in glucose regulation.
Implications for Diabetes Treatment
The implications of this research are significant. Currently, most GLP-1 is produced in the gut, but this study confirms that pancreatic alpha cells can also release GLP-1 into the bloodstream. This process occurs after eating and is essential for controlling blood sugar levels by increasing insulin and decreasing glucagon.
Interestingly, common metabolic stressors, such as a high-fat diet, have been shown to modestly increase GLP-1 production in alpha cells. This discovery opens the door to future research: scientists may be able to find safe methods to enhance GLP-1 output from alpha cells, potentially leading to more effective diabetes treatments.
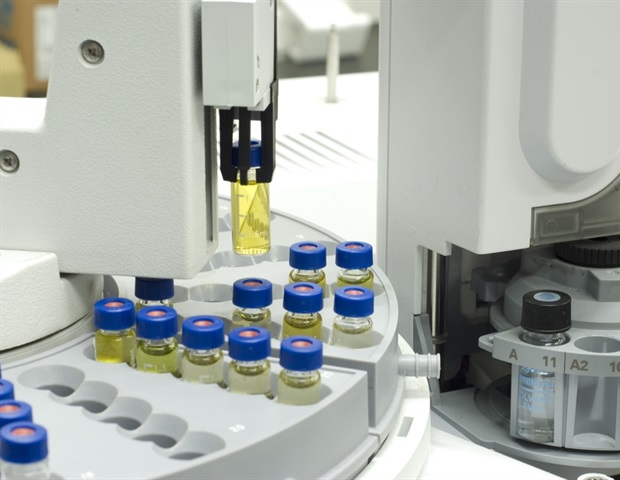
Challenges in Measuring GLP-1
Measuring GLP-1 levels accurately has historically been a challenge due to the presence of inactive GLP-1 fragments that can obscure results. The Duke team overcame this hurdle by developing a high-specificity mass spectrometry assay that detects only the bioactive form of GLP-1, which is crucial for stimulating insulin secretion.
This advancement is vital for further research into GLP-1's role in diabetes management, as it allows for more precise assessments of hormone activity and effectiveness in patients.
A Built-in Backup Plan for Blood Sugar Control
Dr. Campbell remarked, “This discovery shows that the body has a built-in backup plan. GLP-1 is simply a much more powerful signal for beta cells than glucagon.” The ability of alpha cells to switch from glucagon to GLP-1 production during times of metabolic stress may be a critical mechanism through which the body maintains blood sugar control.
As research continues to evolve, the potential for therapies that harness this newfound understanding of pancreatic function could revolutionise treatment options for individuals living with type 2 diabetes.
Conclusion: What Lies Ahead in Diabetes Research
The findings from Duke University challenge long-standing perspectives on blood sugar regulation, highlighting the dual role of pancreatic alpha cells and the importance of GLP-1 in insulin secretion. As scientists continue to explore these mechanisms, there may be opportunities to develop new treatments that naturally enhance GLP-1 production, providing patients with more effective and holistic management strategies for type 2 diabetes.
With future studies focusing on safely boosting GLP-1 output from alpha cells, the landscape of diabetes treatment could witness significant advancements. As we look ahead, the integration of this knowledge into clinical practice could lead to improved outcomes for millions affected by this chronic illness.
How can this new understanding of pancreatic function change the way we approach diabetes treatment? #DiabetesResearch #GLP1 #Type2Diabetes
FAQs
What is the role of pancreatic alpha cells in blood sugar regulation?
Pancreatic alpha cells produce glucagon, which raises blood sugar levels. Recent research indicates they also produce GLP-1, a hormone that enhances insulin secretion and helps regulate glucose levels.
How does GLP-1 affect insulin secretion?
GLP-1 stimulates insulin release from beta cells in the pancreas, lowers blood sugar levels, and inhibits glucagon release, making it essential for glucose metabolism.
What are the implications of the Duke University study for diabetes treatment?
This study suggests that boosting the body's GLP-1 production could provide a more natural way to support insulin levels and manage blood sugar in people with type 2 diabetes.
How was the new method for measuring GLP-1 developed?
The Duke research team created a high-specificity mass spectrometry assay that detects only the bioactive form of GLP-1, allowing for more accurate assessments of its role in insulin secretion.
What future research directions could arise from this study?
Future research may focus on identifying safe methods to enhance GLP-1 production from pancreatic alpha cells, which could lead to new, effective treatments for type 2 diabetes.

:quality(70):focal(913x601:923x611)/cloudfront-us-east-1.images.arcpublishing.com/shawmedia/GQUWWODJ3VDVXDIKIMHSYD7TJI.jpg)
:quality(70)/cloudfront-us-east-1.images.arcpublishing.com/shawmedia/PXG6YDQFBBAHPDZOY3AD2I6KRI.png)
